What is Capnography?
”Capnography is a vital monitor of airway patency and of alveolar ventilation. The importance and breadth of its role has only become apparent recently.”
Association of Anaesthetists - Guideline (May 2021)
What is Capnography?
Capnography is the non-invasive real-time measurement, during inspiration and expiration, of the partial pressure of CO₂ from the airway. It provides continuous physiological information on ventilation, perfusion, and metabolism vital to proper airway management[1]. This enables the identification of adverse events[2] such as airway obstruction, hyperventilation (rapid or deep breathing), hypoventilation
(slow
or shallow breathing) or apnoea (temporary cessation of breathing).
Capnography continuously displays and monitors End-tidal Carbon Dioxide (EtCO₂₂) levels. The combination of a numerical value of EtCO₂ and a capnogram (or real-time CO₂ waveform) enhances its clinical value beyond capnometry, which displays CO₂ in numeric form only.
What is End-tidal
Carbon Dioxide?
End-tidal Carbon Dioxide (EtCO₂) is the level of carbon dioxide released at the end of an exhaled breath. It reflects the adequacy with which CO₂ is circulated and exhaled. Adequate levels of CO₂ are around 35-45 mm Hg.
Why is EtCO₂ important?
Evidence suggests it indicates cardiac output and pulmonary blood flow[7].
Use of capnography is recommended “for all patients, of all ages, and in all locations.”
Association of Anaesthetists - Guideline (May 2021)
Capnography is attracting headlines in medical literature, with Guidelines and International Standards including it as a highly recommended or essential patient safety monitoring[3].
The clinical use of capnography extends to a range of settings both inside and outside of the operating room, including monitoring the effectiveness of CPR, during emergency transportation, in ICU/ITU, in the emergency room, and to ensure the correct placement of an endotracheal tube[4].
Capnography is the most widely recommended method for monitoring EtCO₂ and the optimal method of continuously monitoring the adequacy of ventilation and circulation in infant, paediatric, and adult patients[5],[6].
Indications and Applications of Capnography
Capnography is considered the gold standard measurement for respiratory rate monitoring[8] and it has a range of other clinical applications including monitoring metabolism and circulation[9].
A Guideline published in May 2021 by the Association of Anaesthetists states that waveform capnography should be used for monitoring the airway during anaesthesia, wherever anaesthesia takes place and until a patient has fully recovered from anaesthesia.
Recommendations for the use of capnography from The Association of Anaesthetists:
- Whenever a patient is sedated from induction to recovery
- Where there is a loss of response to verbal contact
- When transferring patients
- With patients who have tracheal tubes and supraglottic airway devices, until these
are removed
Guideline from the Association of Anaesthetists (May 2021)[10]
Additional Monitoring Roles
The Guideline also advises using capnography during lighter levels of sedation to aid monitoring of airway patency, respiratory rate, and pattern[11]. And specifically, to:
- Detect bronchospasm or other lung pathology
- Monitor rebreathing of carbon dioxide
- Signal alterations in metabolic status such as malignant hyperthermia
Guideline from the Association of Anaesthetists (May 2021)[12]
Types of Capnography:
Sidestream – often used in non-intubated patients during procedural sedation, emergency transport and post-operative wake up (i.e. outside the OR)
Microstream – a variation of sidestream capnography used for intubated and non-intubated patients, providing more accurate EtCO₂ measurements[16].
Mainstream – used mainly in the operating room (OR) with intubated patients
How Does a Capnograph Work?
Capnography is monitored via a sampling line that captures exhaled breath from the patient’s nose or mouth. Next, the CO₂ passes through a sensor located at the airways tubing outside the nose/mouth or in a separate analysis chamber. Here, a beam of infrared light passes over the gas, and CO₂ levels are detected.
CO₂ absorbs infrared light at a specific wavelength. Therefore, high infrared light passing to the detector means low levels of CO₂
is present and low infrared light to the sensor means high levels of CO₂. The increase and decrease of CO₂ concentration over time during respiration are translated on to a capnogram.
Benefits of Capnography
CO₂ alerts from capnography monitoring mean medical teams are quickly able to:
- Identify potential breathing complications (e.g., airway obstruction, hyperventilation, hypoventilation, or apnoea) at an early stage
- Respond and intervene accordingly (e.g., by providing supplementary oxygen)
- Help reduce the risk of poor patient outcomes[13]
A Guideline published in May 2021 by the Association of Anaesthetists also highlights the sensitivity and specificity of waveform capnography. These features are not found in other methods of detecting correct intubation, such as palpation and auscultation[14].
How are EtCO₂ Levels Measured in Capnography?
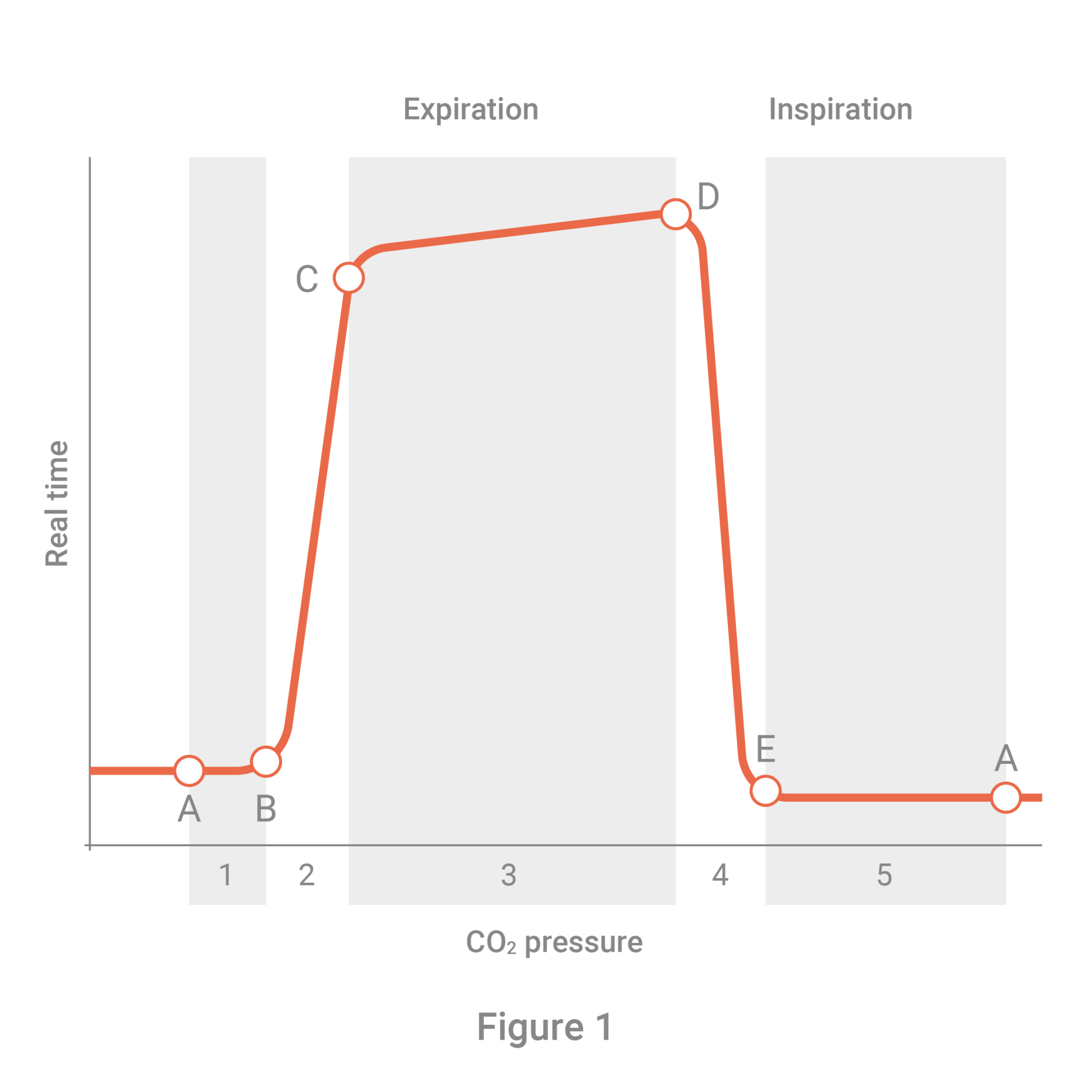
The capnogram displays the 4 phases of the respiratory cycle in a waveform.
Phase I (A-B)
Occurs during inspiration. This is also known as the baseline (A to B). There is no CO₂ because the gas that first passes the sensor is O₂; thus, CO₂ is zero or very low. With no gas exchange, this is also known as ‘dead space’.
Phase 2 (B-C)
Also referred to as the ascending or early expiration phase (B to C). Here CO₂ rises with a small apparent delay. CO₂ rich gas from the lung’s alveolar reaches the upper airways and mixes with the dead air space (in Phase I). This causes a rapid increase in CO₂ levels, detected by the capnogram in exhaled air.
Phase 3 (C-D)
Occurs during late expiration (C to D). This involves the continuous movement of CO₂ across the sensor, resulting in the straight line on the capnogram (the alveolar plateau).
Phase 4 (D-E)
Starts at the end of the alveolar plateau. Here the EtCO₂, which represents the highest CO₂ value, is measured during the respiratory cycle at point D on the capnogram. This phase also shows the beginning of inspiration with O₂ gas passing through the sensor, and CO₂ value drops rapidly to zero.